
Knee pain what is it, how we diagnose and how we can help you at the Rehab Hub Glasgow
So you have knee pain... in this article, I go through how to go about our diagnosis to then be able to best help you. The most important thing we can do is get your diagnosis right.
The Knee
The knee is a common joint to be injured and to develop chronic pain due to the forces that act across the joint and the mechanics of the joint.
The knee joint itself has little stability inherent in the shape of the bones, making it reliant on muscles, tendons, ligaments, and cartilage for the majority of its stability.
There are many causes of knee pain, and these are broadly divided into pain arising from acute injuries and discomfort arising from overuse or chronic changes.

What we do when we see you
When we first see you, we first need to establish whether your knee pain is an acute episode of pain or whether there have been any similar previous episodes. Next, we will look at whether you can weight-bear and whether and if you could at the time of injury, whether there has been any swelling and whether there have been any episodes of locking or giving way of the knee.
For example, twisting injuries on a planted foot may result in meniscal or ligamentous injuries. Falls from more significant than standing height in a young person (or standing height in an older adult) may result in a fracture. Falls onto the front of the knee may result in a patellar fracture, and it may result in forced flexion.
In the latter, disruption of the extensor mechanism at any level may occur (patellar tendon, patella, quadriceps), typically if you are older, the more proximal the injury. In addition, restricted weight-bearing at the time of review suggests the possibility of a fracture or intraarticular pathology.

Swelling why we want to know
The speed swelling happens gives us vital information and helps with diagnosis. Rapid onset (within a few hours) suggests bleeding in the joint either from an intraarticular ligament tear (e.g. anterior cruciate ligament), an osteochondral injury, or a peripheral (vascularised) meniscal injury.
Swelling that takes time to come up (e.g. overnight) suggests your injury is more likely due to a meniscal tear or synovial irritation. In adults, only the very periphery of the meniscus is vascularised. Hence the majority of meniscal tears in adults do not cause bleeding.
Locking knee
Locking or giving way of the knee suggests a meniscal tear or ligamentous injury. Knee popping out” or “popping out and back in” with an associated change of shape is most likely describing a patellar dislocation.
Anterior (front) knee pain suggests a problem with the patellofemoral joint (large bone-in leg and knee). Typical issues here arise from weak muscles (quadriceps and gluteals. The quadriceps have a critical role in the tracking of the patella), tight muscles (quadriceps, hamstrings, and hip flexors), abnormal limb alignment (torsion of the limb, varus/valgus alignment, flat or high arched feet) or overuse.
Instability of the patella either comes on secondary to damage of restraints after a traumatic patellar dislocation or trochlear dysplasia (the normal groove of the trochlear can be domed rather than grooved in extreme cases). Irritation of the patellofemoral joint may arise from osteoarthritis. Anterior knee pain in combination with a visible localised swelling may be due to infrapatellar or prepatellar bursitis.
Patellar or quadriceps tendinopathy may arise from resisted knee extension activities, such as jumping. Rarer causes include structural abnormalities such as a plica in the knee that rubs on the sides of the femur as the knee flexes and extends.
Medial knee pain
Medial knee pain distal (bellow) to the joint line over the insertion of the hamstrings may be due to a pes anserinus bursitis and is more common in valgus knees.
Lateral knee pain
Lateral knee pain exacerbated by activities such as running with no restriction in range of motion may arise from irritation of the iliotibial band. Medial or lateral joint line pain in patients over the age of 50 is most likely to be due to osteoarthritis.
OA of the knee
The earliest sign of knee osteoarthritis is a restriction in the range of motion, with fixed flexion (bent) deformity. Knee pain secondary to inflammatory arthropathies is less likely to be monoarticular.

The Ottawa knee rules
The Ottawa knee rules guide the likelihood of a fracture and a need for an urgent x-ray. The screening tool was developed because of the need for a fast and accurate way to avoid unnecessary imaging. Imaging does not come without its risks/exposure to radiation and is not always indicated.
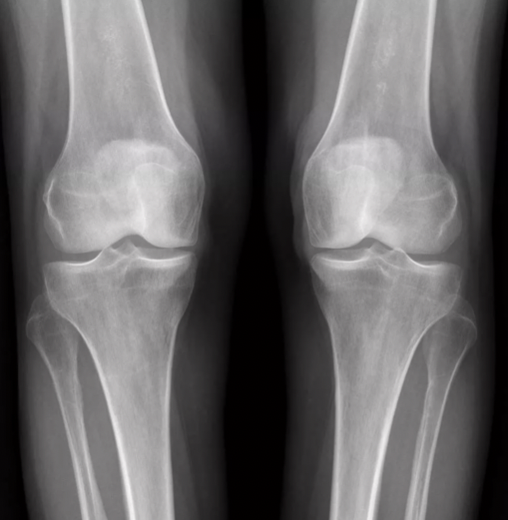
X-ray is recommended if:
Your aged 55 years of age or older
There is isolated patellar tenderness
There is fibular head tenderness
You cannot flex the knee beyond 90 degrees
You were unable to bear weight at the time of injury and is unable to do so at the time of assessment
Common conditions/injuries of the knee
Meniscal tears
- Typically caused by twisting injuries, they can occur on the medial or lateral side.
- Acute traumatic tears in patients under the age of 40 that are symptomatic may need repair or meniscectomy.
- Over the age of 40 years, tears are much more likely to be degenerative. There is evidence that meniscectomy makes no difference to outcomes if the tear is degenerative. The exception to this may be patients with locking and giving way that is restricting their activities.
- On examination, patients have joint line tenderness and irritation on loading of that side of the joint.
- If the knee is locked with a traumatic non-degenerative meniscal tear, then you would expect to be given an urgent referral to an acute knee clinic or a fracture clinic. In this situation, there may be a displaced bucket handle tear causing the locking, which needs to be put back into place and repaired. The longer these are left, the more likely they are to be irreparable due to plastic deformation of the torn bit of meniscus.
Anterior cruciate ligament (ACL) tears
- When an ACL tear happens, it is typically associated with an episode of significant trauma.
- Cutting and pivoting motions are common mechanisms of injury.
- Following injury, you typically struggle to weight-bear, and there is a rapid onset effusion (swelling).
- Patients often complain of knee instability or a loss of confidence in the knee, particularly going up or downstairs.
- Early intervention with MSK Podiatry or Physiotherapy is beneficial as not all patients with a ruptured ACL require reconstruction (the main indication for referral for reconstruction is recurrent instability).
Medial or lateral collateral ligament tear
- Typically sustained during a varus or valgus strain to the knee, such as an impact on the side of a loaded knee.
- There is either pain or opening up of the knee when varus or valgus stress is applied – this is done with the knee in 10 to 20 degrees of flexion. In full extension, the ACL acts as a secondary stabiliser.
Iliotibial band (ITB) syndrome
- Known as runner’s knee
- Lateral sided knee pain with tenderness where the ITB runs over the lateral femoral
- condyle
- Commonly associated with pain over the greater trochanter at the level of tensor
- fascia latae
Osteoarthritis
- Common over the age of 50
- Symptoms of pain, stiffness and restriction of activities of daily living
- Management – exercise (stay active as much as possible), weight loss, analgesia, intraarticular injections, offloader braces (if only one compartment affected), osteotomy, and joint replacement
We will always consider the possibility of septic arthritis, for which the knee is acutely painful with a very restricted range of motion. For chronic problems, advice regarding analgesia, exercises, and activity modification in the first instance.
We have many treatments available in our clinic. From injection therapy including PRP, Shockwave Therapy, Laser Therapy, Exercise Rehab, Gait retraining, manipulation, soft tissue therapy, and more. The first thing we need to establish is a working diagnosis - from there we will be best placed to help you.
If your pain is coming on after you walk/run and seems to be more chronic in nature we would recommend musculoskeletal assessment via our 3D assessment.
To book a full 3D MSK assessment - please click here
Would you like to discuss your needs with us? Book a FREE in person or over the phone consultation.




